Crucial Insights into COPD: Unraveling the Respiratory Conundrum
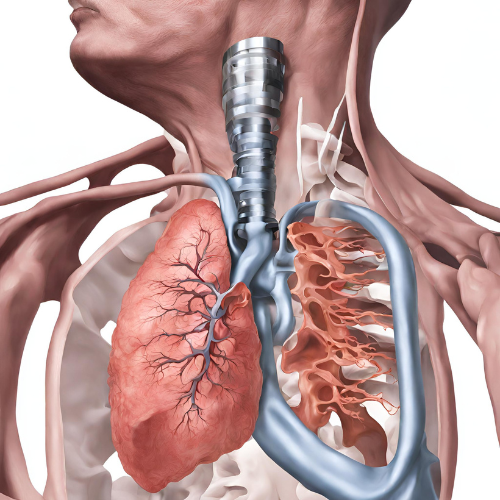
What is COPD? Chronic Obstructive Pulmonary Disease (COPD) is a progressive lung disease characterized by persistent airflow limitation and difficulty breathing. This condition encompasses various respiratory ailments, including chronic bronchitis and emphysema, and is typically associated with long-term exposure to irritating gases or particulate matter, such as cigarette smoke.
Types of COPD: COPD encompasses two primary conditions:
- Chronic Bronchitis: Inflammation and narrowing of the airways, leading to excessive mucus production and persistent cough.
- Emphysema: Damage to the air sacs in the lungs (alveoli), resulting in reduced lung elasticity and impaired gas exchange.
Symptoms of COPD: Common symptoms of COPD include:
- Persistent cough, often with mucus (sputum) production.
- Shortness of breath, especially during physical activity.
- Wheezing or chest tightness.
- Fatigue and decreased exercise tolerance.
- Frequent respiratory infections.
- Bluish tint to the lips or fingernails (cyanosis) in advanced cases.
Causes of COPD: COPD is primarily caused by exposure to harmful substances that damage the lungs over time, such as:
- Cigarette smoke (including secondhand smoke).
- Occupational exposure to dust, chemicals, or fumes.
- Indoor air pollution from biomass fuels (e.g., wood or coal).
- Genetic factors, including alpha-1 antitrypsin deficiency (a rare genetic disorder).
Risk Factors for COPD: Several factors may increase the risk of developing COPD, including:
- Smoking: Tobacco smoke is the leading cause of COPD, accounting for the majority of cases.
- Occupational exposure: Certain occupations, such as mining, construction, or agriculture, pose a higher risk of lung damage due to exposure to dust or chemicals.
- Age: COPD is more common in older adults, particularly those over 40 years of age.
- Genetics: Individuals with a family history of COPD or alpha-1 antitrypsin deficiency are at increased risk.
- Respiratory infections: Chronic respiratory infections, especially during childhood, may contribute to the development of COPD later in life.
Diagnosis of COPD: Diagnosis of COPD typically involves a combination of medical history, physical examination, and diagnostic tests, including:
- Pulmonary function tests (spirometry) to measure lung function and airflow limitation.
- Chest X-ray or CT scan to evaluate lung structure and detect abnormalities.
- Arterial blood gas analysis to assess oxygen and carbon dioxide levels in the blood.
- Assessment of symptoms and risk factors, including smoking history and occupational exposures.
Pharmacokinetics and Pharmacodynamics: Pharmacological treatment for COPD aims to alleviate symptoms, improve lung function, and reduce the risk of exacerbations. These medications may vary in their absorption, distribution, metabolism, and excretion, as well as their mechanisms of action within the body.
Pharmacological Treatment: a. Bronchodilators: These medications relax the muscles around the airways, making it easier to breathe. They include short-acting bronchodilators (e.g., albuterol) for immediate relief and long-acting bronchodilators (e.g., tiotropium) for maintenance therapy. b. Inhaled Corticosteroids: These medications help reduce airway inflammation and may be used in combination with bronchodilators for moderate to severe COPD. c. Phosphodiesterase-4 Inhibitors: These medications reduce inflammation and may be used in patients with severe COPD and chronic bronchitis who have frequent exacerbations.
Non-Pharmacological Treatment: a. Smoking cessation: Quitting smoking is the single most effective way to slow the progression of COPD and improve lung function. b. Pulmonary rehabilitation: This comprehensive program includes exercise training, education, and support to help individuals with COPD improve their symptoms and quality of life. c. Oxygen therapy: Supplemental oxygen therapy may be prescribed for patients with severe COPD and low blood oxygen levels to improve breathing and reduce the risk of complications.
Conclusion: COPD is a progressive lung disease characterized by persistent airflow limitation and difficulty breathing. While there is no cure for COPD, early diagnosis and appropriate management can help slow the progression of the disease, relieve symptoms, and improve quality of life. If you experience symptoms of COPD or are at risk due to smoking or occupational exposures, it’s essential to seek medical evaluation and guidance for proper diagnosis and treatment. With a comprehensive approach that includes pharmacological and non-pharmacological interventions, individuals with COPD can achieve better symptom control and enjoy a higher quality of life.