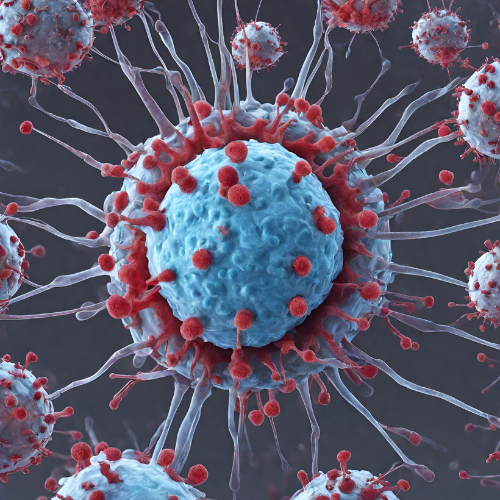
Unraveling the Complexities of COVID-19 Complications: A Comprehensive Overview
As the COVID-19 pandemic continues to evolve, researchers and healthcare professionals are gaining a deeper understanding of the various complications associated with this viral illness. While COVID-19 primarily affects the respiratory system, it can also lead to a wide range of complications affecting multiple organs and systems in the body. In this comprehensive overview, we delve into the diverse array of COVID-19 complications, from respiratory issues to cardiovascular, neurological, and beyond.
Respiratory Complications:
- Pneumonia: COVID-19 can cause severe pneumonia characterized by inflammation and fluid buildup in the lungs, leading to respiratory distress and difficulty breathing.
- Acute Respiratory Distress Syndrome (ARDS): In severe cases, COVID-19 can trigger ARDS, a life-threatening condition marked by widespread inflammation in the lungs, impaired oxygen exchange, and respiratory failure.
- Respiratory Failure: Severe COVID-19 pneumonia and ARDS can result in respiratory failure, necessitating mechanical ventilation and intensive care support.
Cardiovascular Complications:
- Myocarditis: COVID-19 can cause inflammation of the heart muscle (myocarditis), leading to chest pain, arrhythmias, and heart failure.
- Acute Coronary Syndrome: Individuals with COVID-19 may be at increased risk of acute coronary syndrome, including myocardial infarction (heart attack) and unstable angina.
- Thromboembolic Events: COVID-19 is associated with an increased risk of blood clotting disorders, leading to deep vein thrombosis (DVT), pulmonary embolism (PE), and stroke.
Neurological Complications:
- Encephalopathy: COVID-19 can lead to altered mental status, confusion, and encephalopathy, particularly in older adults and those with pre-existing neurological conditions.
- Stroke: COVID-19 is associated with an increased risk of ischemic stroke, hemorrhagic stroke, and cerebral venous sinus thrombosis.
- Guillain-Barré Syndrome (GBS): Rare cases of GBS, a neurological disorder characterized by progressive muscle weakness and paralysis, have been reported following COVID-19 infection.
Renal Complications:
- Acute Kidney Injury (AKI): COVID-19 can cause AKI, a sudden loss of kidney function, leading to electrolyte imbalances, fluid overload, and the need for renal replacement therapy.
- Renal Thrombotic Microangiopathy: COVID-19-associated renal thrombotic microangiopathy is characterized by thrombosis in the small blood vessels of the kidneys, leading to kidney dysfunction and injury.
Gastrointestinal Complications:
- Acute Liver Injury: COVID-19 can cause liver inflammation and injury, manifesting as elevated liver enzymes, jaundice, and hepatomegaly.
- Gastrointestinal Bleeding: COVID-19 is associated with an increased risk of gastrointestinal bleeding, particularly in critically ill patients receiving anticoagulant therapy.
Hematological Complications:
- Disseminated Intravascular Coagulation (DIC): Severe COVID-19 can trigger DIC, a life-threatening condition characterized by widespread blood clotting and simultaneous bleeding.
- Hemophagocytic Lymphohistiocytosis (HLH): COVID-19-associated HLH is a rare but serious complication characterized by excessive immune activation and systemic inflammation.
Long COVID: Many individuals who recover from acute COVID-19 continue to experience lingering symptoms for weeks or months, a condition commonly referred to as “long COVID” or “post-acute sequelae of SARS-CoV-2 infection” (PASC). Common long COVID symptoms include fatigue, shortness of breath, cognitive impairment (“brain fog”), and musculoskeletal pain.
Conclusion: The spectrum of COVID-19 complications is vast and multifaceted, encompassing respiratory, cardiovascular, neurological, renal, gastrointestinal, hematological, and other systemic manifestations. As our understanding of COVID-19 continues to evolve, ongoing research efforts are crucial for elucidating the underlying mechanisms of these complications and developing targeted interventions to improve outcomes for individuals affected by this devastating disease. By recognizing and addressing the diverse array of COVID-19 complications, healthcare providers can provide comprehensive care and support to patients throughout their illness trajectory.