Understanding Edema: Types, Symptoms, Causes, and Treatment
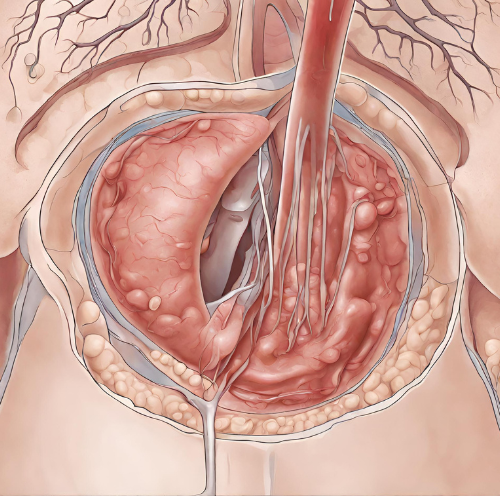
What is Edema? Edema is a medical term used to describe the abnormal accumulation of fluid in the body’s tissues, leading to swelling and enlargement of affected areas. It can occur in various parts of the body, including the legs, feet, ankles, hands, arms, lungs, and abdomen. Edema is often a symptom of an underlying health condition and can range from mild to severe.
Types of Edema:
- Peripheral Edema: Swelling in the extremities, such as the legs, feet, hands, or arms.
- Pulmonary Edema: Accumulation of fluid in the lungs, leading to difficulty breathing, coughing, and wheezing.
- Cerebral Edema: Swelling of the brain tissue, which can result from traumatic brain injury, stroke, or brain tumors.
- Macular Edema: Fluid buildup in the macula, the central part of the retina, which can affect vision and lead to vision loss.
Symptoms of Edema:
- Swelling: Visible swelling or puffiness in the affected area.
- Pitting Edema: Pressing on the swollen area leaves an indentation (pit) that persists for a few seconds or minutes.
- Tightness or Heaviness: Sensation of tightness or heaviness in the affected limb or body part.
- Decreased Range of Motion: Difficulty moving the affected joint or limb due to swelling.
- Shortness of Breath: In cases of pulmonary edema, difficulty breathing, especially when lying down or exerting oneself.
Causes and Risk Factors:
- Fluid Retention: Conditions that disrupt the body’s fluid balance, such as heart failure, kidney disease, liver cirrhosis, or venous insufficiency, can lead to edema.
- Inflammation: Inflammatory conditions such as arthritis, dermatitis, or infections can cause localized swelling and edema.
- Medications: Certain medications, including corticosteroids, nonsteroidal anti-inflammatory drugs (NSAIDs), calcium channel blockers, and estrogen-containing drugs, may cause fluid retention and edema as side effects.
- Pregnancy: Hormonal changes and increased pressure on blood vessels during pregnancy can lead to fluid retention and edema, especially in the legs and feet.
- Lifestyle Factors: Prolonged standing or sitting, excessive salt intake, poor circulation, and obesity can contribute to the development of edema.
Diagnosis: Diagnosis of edema typically involves a medical history review, physical examination, and assessment of symptoms. Additional tests, such as blood tests, urine tests, imaging studies (ultrasound, CT scan, MRI), or echocardiography, may be ordered to identify underlying causes or assess organ function.
Pathophysiology: The pathophysiology of edema involves an imbalance between fluid movement into and out of the body’s tissues. Normally, fluid is filtered out of the bloodstream into the interstitial spaces by capillaries and lymphatic vessels, and then returned to the bloodstream via lymphatic drainage. However, when there is an increase in capillary pressure, leakage of fluid from capillaries, decreased oncotic pressure, or impaired lymphatic drainage, excess fluid accumulates in the tissues, leading to edema.
Pharmacological Treatment:
- Diuretics: Medications such as loop diuretics (furosemide), thiazide diuretics (hydrochlorothiazide), or potassium-sparing diuretics (spironolactone) may be prescribed to increase urine output and reduce fluid retention in cases of edema.
- Angiotensin-Converting Enzyme (ACE) Inhibitors: ACE inhibitors, such as lisinopril or enalapril, may be used to treat edema associated with heart failure or kidney disease by reducing blood pressure and improving heart function.
- Calcium Channel Blockers: Medications like amlodipine or nifedipine can help relax blood vessels and reduce blood pressure, thus alleviating edema in cases of venous insufficiency or hypertension.
Non-Pharmacological Treatment:
- Compression Therapy: Wearing compression stockings or sleeves can help improve circulation and reduce swelling in the legs or arms.
- Elevation: Elevating the affected limb above the level of the heart can help promote fluid drainage and reduce swelling.
- Dietary Changes: Limiting salt intake, increasing potassium-rich foods, staying hydrated, and following a balanced diet can help manage fluid retention and reduce edema.
- Exercise: Regular physical activity can improve circulation, reduce fluid buildup, and prevent edema.
Conclusion: Edema is a common condition characterized by the abnormal accumulation of fluid in the body’s tissues, leading to swelling and discomfort. While mild edema may resolve on its own or with conservative management, persistent or severe edema may require medical intervention to identify and address underlying causes. Understanding the types, symptoms, causes, and treatment options for edema is essential for effectively managing this condition and improving quality of life. Individuals experiencing persistent or worsening symptoms of edema should seek medical evaluation and treatment to prevent complications and address underlying health concerns.