Understanding Epilepsy: Pathophysiology, Pharmacokinetics, Pharmacodynamics, and Treatment
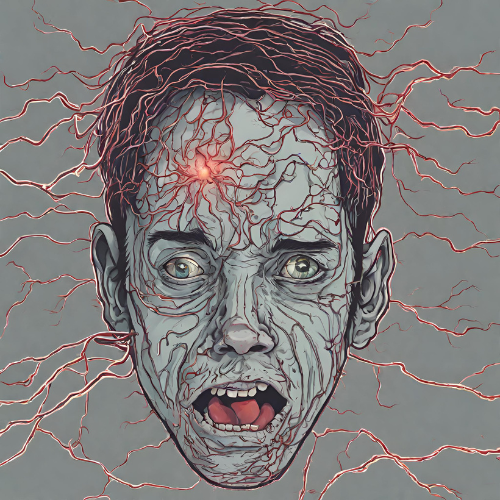
What is Epilepsy? Epilepsy is a chronic neurological disorder characterized by recurrent seizures, which are sudden, unprovoked electrical disturbances in the brain. Seizures can vary widely in severity and manifestation, ranging from brief lapses of consciousness to convulsions involving involuntary movements and loss of awareness. Epilepsy can affect people of all ages and may have various causes, including genetic factors, brain injuries, infections, and developmental disorders.
Pathophysiology of Epilepsy:
- Abnormal Brain Activity: In individuals with epilepsy, the normal electrical activity of the brain is disrupted, leading to hyperexcitability and hyper synchronization of neuronal firing.
- Seizure Generation: Seizures result from sudden, excessive electrical discharges in specific areas of the brain, which can spread and involve other regions, leading to the characteristic signs and symptoms observed during a seizure.
- Epileptogenesis: The process by which normal brain tissue becomes hyperexcitable and prone to recurrent seizures is known as epileptogenesis. This may involve changes in ion channel function, neurotransmitter imbalance, or alterations in neuronal connectivity.
Pharmacokinetics (PK) and Pharmacodynamics (PD):
- Pharmacokinetics: Antiepileptic drugs (AEDs) exhibit diverse pharmacokinetic profiles, including absorption, distribution, metabolism, and excretion. Individual variability in drug absorption and metabolism can influence drug efficacy and tolerability.
- Pharmacodynamics: AEDs exert their pharmacodynamic effects by modulating neuronal excitability, neurotransmitter release, or ion channel function in the brain. Common mechanisms of action include enhancing gamma-aminobutyric acid (GABA)ergic inhibition, blocking voltage-gated sodium channels, or reducing glutamatergic excitatory transmission.
Treatment of Epilepsy:
- Antiepileptic Drugs (AEDs): The primary treatment for epilepsy involves the use of AEDs to prevent or reduce the frequency and severity of seizures. A wide range of AEDs are available, each with unique mechanisms of action and side effect profiles. Examples include:
- First-line AEDs: Carbamazepine, phenytoin, valproic acid, and levetiracetam.
- Newer AEDs: Lamotrigine, topiramate, oxcarbazepine, and lacosamide.
- Surgical Intervention: For individuals with drug-resistant epilepsy or focal seizures originating from a specific area of the brain, surgical resection of the epileptic focus may be considered.
- Vagus Nerve Stimulation (VNS): VNS involves implanting a device that delivers electrical stimulation to the vagus nerve, which can help reduce seizure frequency and severity in some patients.
- Ketogenic Diet: The ketogenic diet, a high-fat, low-carbohydrate diet that mimics the metabolic effects of fasting, has been shown to be effective in reducing seizures, particularly in children with drug-resistant epilepsy.
- Lifestyle Modifications: Avoiding triggers such as sleep deprivation, stress, or alcohol consumption, maintaining a regular sleep schedule, and adhering to medication regimens are essential aspects of managing epilepsy.
Conclusion: Epilepsy is a complex neurological disorder characterized by recurrent seizures and diverse underlying causes. Understanding the pathophysiology, pharmacokinetics, and pharmacodynamics of antiepileptic drugs is crucial for optimizing treatment outcomes and improving quality of life for individuals living with epilepsy. While AEDs are the cornerstone of epilepsy management, surgical interventions, neuromodulation techniques, and lifestyle modifications play important adjunctive roles in controlling seizures and reducing the burden of epilepsy on affected individuals and their families. Ongoing research into novel treatment approaches and personalized therapeutic strategies holds promise for further advances in epilepsy care and management. Early diagnosis, comprehensive evaluation, and individualized treatment plans tailored to each patient’s unique needs are essential for achieving optimal seizure control and improving long-term prognosis in epilepsy.