Understanding Hyperparathyroidism: Causes, Symptoms, and Management
Introduction to Hyperparathyroidism: Hyperparathyroidism is a condition characterized by the overactivity of the parathyroid glands, resulting in excessive production of parathyroid hormone (PTH). This hormone regulates calcium levels in the blood and plays a crucial role in maintaining bone health. When the parathyroid glands produce too much PTH, it can lead to elevated calcium levels in the blood (hypercalcemia) and various health complications. Understanding the causes, symptoms, and management of hyperparathyroidism is essential for effective treatment and prevention of complications.
Causes of Hyperparathyroidism:
- Primary Hyperparathyroidism: This occurs when one or more of the parathyroid glands become overactive and produce too much PTH. The exact cause is often unknown but may be due to a benign tumor (adenoma) on one of the glands or, less commonly, hyperplasia of multiple glands.
- Secondary Hyperparathyroidism: This type of hyperparathyroidism develops as a result of another underlying condition, such as chronic kidney disease, vitamin D deficiency, or malabsorption disorders. In secondary hyperparathyroidism, the overactivity of the parathyroid glands is a compensatory response to low calcium levels or impaired calcium metabolism.
- Tertiary Hyperparathyroidism: In some cases, secondary hyperparathyroidism can progress to tertiary hyperparathyroidism, where the parathyroid glands become autonomously overactive, independent of the underlying cause.
Symptoms of Hyperparathyroidism:
- Fatigue and Weakness: Excessive levels of calcium in the blood can cause fatigue, weakness, and overall lethargy.
- Bone Pain: Hyperparathyroidism can lead to bone loss and increased risk of fractures, resulting in bone pain, especially in the ribs, back, and hips.
- Kidney Stones: Elevated calcium levels can increase the risk of developing kidney stones, leading to symptoms such as severe abdominal or flank pain, nausea, and vomiting.
- Digestive Issues: Hypercalcemia can cause gastrointestinal symptoms such as nausea, vomiting, constipation, and loss of appetite.
- Muscle Weakness: High calcium levels may affect muscle function, leading to weakness, cramps, and spasms.
- Excessive Thirst and Urination: Increased calcium levels can stimulate excessive thirst (polydipsia) and frequent urination (polyuria).
- Mental Confusion: Severe hypercalcemia can affect cognitive function, causing confusion, memory problems, and difficulty concentrating.
- Depression and Anxiety: Changes in calcium levels may also affect mood, leading to symptoms of depression, anxiety, or irritability.
Diagnosis of Hyperparathyroidism:
- Blood Tests: Blood tests to measure calcium, PTH, and vitamin D levels are essential for diagnosing hyperparathyroidism.
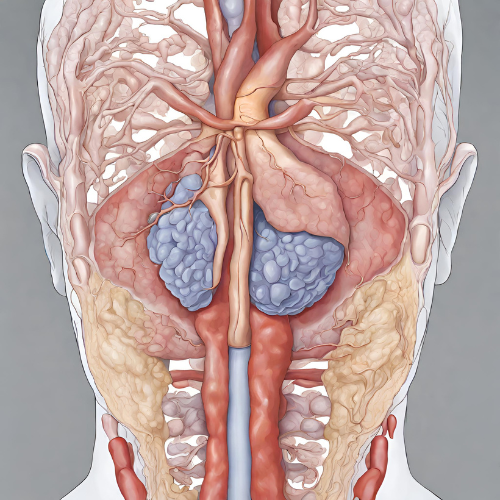
- Imaging Studies: Imaging tests such as ultrasound, sestamibi scan, or MRI may be performed to locate any abnormalities or tumors in the parathyroid glands.
- Bone Density Scan: A bone density scan (DEXA scan) may be recommended to assess bone density and detect signs of osteoporosis or bone loss.
- 24-Hour Urine Collection: Collecting urine over a 24-hour period can help assess calcium excretion and detect the presence of kidney stones.
Management of Hyperparathyroidism:
- Monitoring and Observation: In some cases, especially if hyperparathyroidism is mild or asymptomatic, a watch-and-wait approach may be recommended with regular monitoring of calcium and PTH levels.
- Medications: Medications such as calcimimetics (e.g., cinacalcet) or bisphosphonates may be prescribed to help lower calcium levels and prevent bone loss.
- Surgery (Parathyroidectomy): Surgical removal of the affected parathyroid gland(s) may be necessary, particularly in cases of primary hyperparathyroidism with severe symptoms, complications, or evidence of kidney damage.
- Fluids and Hydration: Drinking plenty of fluids can help prevent dehydration and reduce the risk of kidney stone formation.
- Calcium and Vitamin D Supplementation: In cases of vitamin D deficiency or inadequate calcium intake, supplementation may be recommended to support bone health and calcium metabolism.
- Lifestyle Modifications: Adopting a healthy lifestyle, including regular exercise, a balanced diet rich in calcium and vitamin D, and avoiding excessive alcohol and caffeine intake, can help manage hyperparathyroidism and reduce the risk of complications.
Conclusion: Hyperparathyroidism is a condition characterized by excessive production of parathyroid hormone, leading to elevated calcium levels in the blood and various health complications. Early diagnosis and appropriate management are crucial for preventing complications such as kidney stones, osteoporosis, and kidney damage. Treatment options may include medications, surgery, fluid management, and lifestyle modifications to help restore calcium balance and improve overall health and well-being. Regular monitoring and follow-up with a healthcare provider are essential for managing hyperparathyroidism effectively and preventing long-term complications.