Understanding Hypoparathyroidism: Causes, Symptoms, and Management
Introduction to Hypoparathyroidism: Hypoparathyroidism is a rare endocrine disorder characterized by insufficient production or activity of parathyroid hormone (PTH) by the parathyroid glands. PTH plays a crucial role in regulating calcium and phosphorus levels in the blood. When PTH levels are low, it can lead to decreased calcium levels (hypocalcemia) and increased phosphorus levels (hyperphosphatemia), resulting in various symptoms and complications. Understanding the causes, symptoms, and management of hypoparathyroidism is essential for effective treatment and improving quality of life for affected individuals.
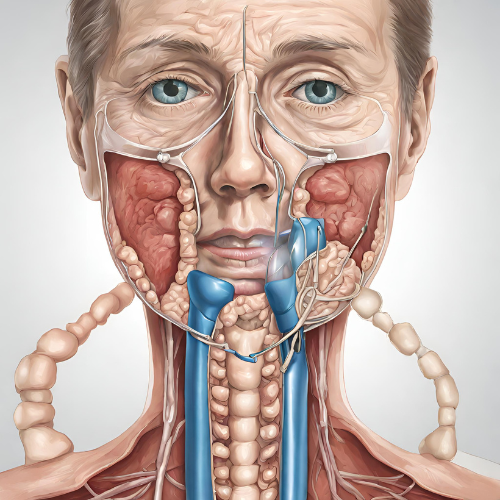
Causes of Hypoparathyroidism:
- Surgical Removal of Parathyroid Glands: The most common cause of hypoparathyroidism is the inadvertent removal or damage to the parathyroid glands during thyroid or neck surgery.
- Autoimmune Conditions: Autoimmune diseases such as autoimmune thyroiditis or autoimmune polyendocrine syndrome type 1 can result in destruction or dysfunction of the parathyroid glands.
- Genetic Factors: Rare genetic disorders, such as DiGeorge syndrome or familial isolated hypoparathyroidism, can lead to congenital hypoparathyroidism.
- Hypomagnesemia: Low magnesium levels can impair PTH secretion and contribute to hypoparathyroidism.
- Radiation Therapy: Neck irradiation for the treatment of head and neck cancers can damage the parathyroid glands and lead to hypoparathyroidism.
- Idiopathic: In some cases, the cause of hypoparathyroidism may be unknown (idiopathic).
Symptoms of Hypoparathyroidism:
- Muscle Cramps and Spasms: Hypocalcemia can cause muscle twitching, cramps, and spasms, particularly in the hands, feet, and face.
- Tingling and Numbness: Nerve-related symptoms such as tingling sensations (paresthesia), numbness, and pins-and-needles sensation (paresthesia) may occur, especially in the fingertips, lips, and around the mouth.
- Fatigue and Weakness: Low calcium levels can lead to fatigue, weakness, and lethargy.
- Seizures: Severe hypocalcemia can increase the risk of seizures, which may manifest as tonic-clonic convulsions.
- Mental Confusion: Hypocalcemia can affect cognitive function, causing confusion, memory problems, and difficulty concentrating.
- Depression and Anxiety: Changes in calcium levels may affect mood, leading to symptoms of depression, anxiety, or irritability.
- Dry, Coarse Skin: Hypoparathyroidism can cause dry, coarse skin and brittle nails due to impaired calcium metabolism.
- Cataracts: Chronic hypocalcemia may increase the risk of developing cataracts, leading to blurred vision and visual disturbances.
- Dental Problems: Low calcium levels can affect dental health, leading to tooth enamel defects, increased risk of cavities, and gum disease.
Diagnosis of Hypoparathyroidism:
- Blood Tests: Blood tests to measure calcium, phosphorus, and PTH levels are essential for diagnosing hypoparathyroidism.
- Electrocardiogram (ECG): An ECG may be performed to assess for signs of cardiac arrhythmias or abnormalities associated with hypocalcemia.
- Imaging Studies: Imaging tests such as ultrasound or MRI may be used to evaluate the structure and function of the parathyroid glands.
- Genetic Testing: Genetic testing may be recommended in cases of suspected genetic or familial hypoparathyroidism.
Management of Hypoparathyroidism:
- Calcium and Vitamin D Supplementation: The mainstay of treatment for hypoparathyroidism involves calcium and vitamin D supplementation to raise and maintain calcium levels within the normal range.
- Calcitriol (Active Vitamin D): Calcitriol, a biologically active form of vitamin D, may be prescribed to enhance intestinal absorption of calcium and promote bone mineralization.
- Magnesium Replacement: In cases of hypomagnesemia, magnesium supplementation may be necessary to support PTH secretion and calcium metabolism.
- Monitoring and Follow-Up: Regular monitoring of calcium, phosphorus, and kidney function is essential for adjusting medication doses and assessing treatment response.
- Lifestyle Modifications: Adopting a calcium-rich diet, avoiding excessive phosphorus intake (e.g., from processed foods and carbonated beverages), and maintaining adequate hydration are important for managing hypoparathyroidism.
- Medical Alert Bracelet: Individuals with hypoparathyroidism may benefit from wearing a medical alert bracelet or necklace to notify healthcare providers of their condition in case of emergencies.
Conclusion: Hypoparathyroidism is a complex endocrine disorder characterized by deficient PTH production or activity, leading to hypocalcemia and associated symptoms. Early diagnosis and appropriate management are crucial for preventing complications and optimizing quality of life for individuals with hypoparathyroidism. Close collaboration between patients, healthcare providers, and specialists is essential for developing personalized treatment plans tailored to individual needs and ensuring optimal outcomes.