Jakob-Creutzfeldt Disease, often abbreviated as CJD, is a rare and fatal neurodegenerative disorder that affects the brain. It belongs to a group of diseases known as transmissible spongiform encephalopathies (TSEs), which are characterized by the accumulation of abnormal prion proteins in the brain tissue. CJD can manifest in several forms, including sporadic, familial, and acquired (variant) forms, each with distinct causes and characteristics.
Causes of Jakob-Creutzfeldt Disease (CJD):
- Prion Proteins: CJD is caused by the abnormal folding of prion proteins, leading to the formation of infectious particles called prions. These prions accumulate in the brain, causing neuronal damage and death.
- Sporadic CJD: The majority of CJD cases occur spontaneously without a known cause, termed sporadic CJD. It is believed to result from spontaneous changes in the structure of normal prion proteins.
- Familial CJD: In some cases, CJD may be inherited due to mutations in the PRNP gene, which provides instructions for producing prion proteins. Familial CJD accounts for a small percentage of cases and tends to run in families.
- Acquired (Variant) CJD: Variant CJD is a rare form of the disease that is linked to exposure to contaminated beef products containing abnormal prions, particularly during the bovine spongiform encephalopathy (BSE) epidemic in the late 20th century.
Symptoms of Jakob-Creutzfeldt Disease:
- Rapid Cognitive Decline: CJD typically causes rapid deterioration in cognitive function, including memory loss, confusion, and difficulty concentrating.
- Movement Disorders: Patients may experience muscle stiffness, tremors, jerky movements, and coordination problems.
- Behavioral Changes: Personality changes, mood swings, irritability, and agitation are common symptoms of CJD.
- Vision Problems: Blurred vision, visual disturbances, and blindness may occur as the disease progresses.
- Sleep Disturbances: Insomnia, daytime drowsiness, and disruptions in sleep-wake cycles are often observed.
- Neurological Symptoms: Seizures, sensory disturbances, and speech difficulties may develop as CJD advances.
Diagnosis of Jakob-Creutzfeldt Disease:
- Clinical Evaluation: A thorough medical history, physical examination, and neurological assessment are conducted to evaluate symptoms and detect signs of cognitive decline and neurological abnormalities.
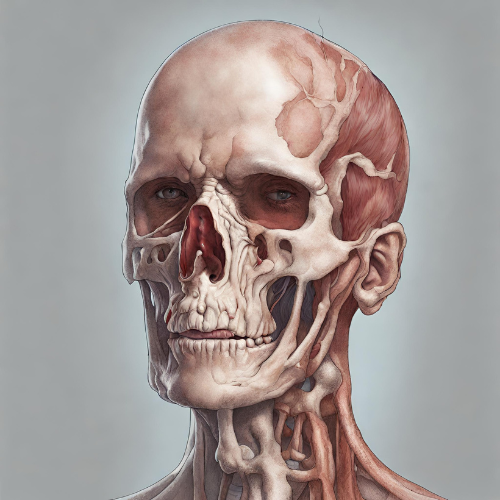
- Brain Imaging: Magnetic resonance imaging (MRI) or computed tomography (CT) scans of the brain may reveal characteristic changes, such as brain atrophy and abnormalities in specific brain regions.
- Cerebrospinal Fluid Analysis: Lumbar puncture (spinal tap) may be performed to analyze cerebrospinal fluid for the presence of abnormal prion proteins.
- Brain Biopsy: In some cases, a brain biopsy may be necessary to confirm the diagnosis by detecting abnormal prion protein accumulation in brain tissue.
Treatment of Jakob-Creutzfeldt Disease:
- Symptomatic Management: Treatment aims to alleviate symptoms and improve the patient’s quality of life through supportive care measures, including medications to manage pain, agitation, and sleep disturbances.
- Experimental Therapies: Various experimental treatments and clinical trials are underway to explore potential therapies targeting abnormal prion proteins and disease progression. However, no curative treatment currently exists for CJD.
- Palliative Care: As CJD is ultimately fatal, palliative care focuses on providing comfort, pain relief, and emotional support to patients and their families throughout the course of the disease.
Management of Jakob-Creutzfeldt Disease:
- Patient and Caregiver Support: Patients with CJD require comprehensive care and support from healthcare professionals, caregivers, and support networks to address their physical, emotional, and psychosocial needs.
- Monitoring and Symptom Management: Regular monitoring of disease progression and symptoms is essential to adjust treatment strategies and optimize symptom management.
- End-of-Life Planning: Advanced care planning and discussions about end-of-life preferences, including palliative care options and hospice services, are important considerations for patients and their families facing a terminal diagnosis.
Conclusion: Jakob-Creutzfeldt Disease is a rare and devastating neurodegenerative disorder characterized by rapid cognitive decline, movement disorders, and neurological symptoms. While there is currently no cure for CJD, early diagnosis, supportive care, and symptom management are crucial for optimizing patient outcomes and quality of life. Continued research into the underlying mechanisms of CJD and the development of innovative therapies are essential for advancing treatment options and improving patient care in the future.