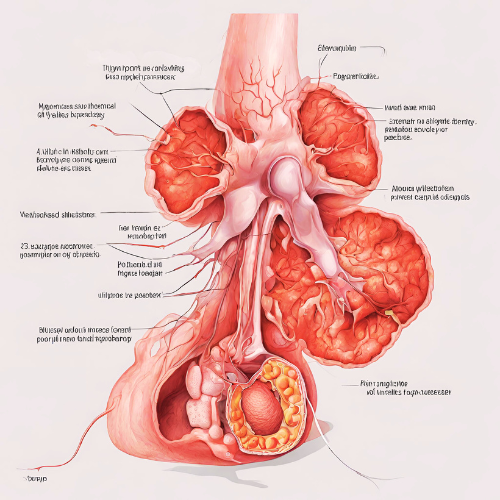
1. What is Pompe’s Disease? Pompe’s disease, also known as glycogen storage disease type II or acid maltase deficiency, is a rare genetic disorder characterized by the buildup of glycogen in cells, particularly muscle cells. This accumulation of glycogen impairs the function of various organs, especially muscles, leading to progressive muscle weakness and other complications.
2. Types of Pompe’s Disease:
- Infantile-onset Pompe’s disease: Begins within the first few months of life and typically presents with severe muscle weakness, enlarged heart (cardiomegaly), and respiratory difficulties.
- Late-onset Pompe’s disease: Develops later in childhood, adolescence, or adulthood and tends to have a milder progression, with muscle weakness primarily affecting the limbs and respiratory muscles.
3. Symptoms of Pompe’s Disease:
- Muscle weakness and fatigue
- Hypotonia (low muscle tone)
- Enlarged heart (cardiomegaly)
- Respiratory problems, such as difficulty breathing and respiratory infections
- Delayed motor milestones (in infants)
- Difficulty swallowing (dysphagia)
- Poor growth and failure to thrive (in infants)
- Progressive muscle weakness, leading to mobility issues and disability
4. Causes of Pompe’s Disease: Pompe’s disease is caused by mutations in the GAA gene, which provides instructions for producing the acid alpha-glucosidase (GAA) enzyme. This enzyme is responsible for breaking down glycogen into glucose, a process essential for providing energy to cells. Mutations in the GAA gene result in deficient or dysfunctional GAA enzyme activity, leading to the accumulation of glycogen in cells.
5. Risk Factors for Pompe’s Disease:
- Family history of Pompe’s disease or carriers of the GAA gene mutation
- Consanguineous (related by blood) parents
- Certain ethnicities, such as individuals of Dutch descent, who have a higher prevalence of Pompe’s disease
6. Diagnosis of Pompe’s Disease:
- Enzyme assay: A blood test measuring the activity of acid alpha-glucosidase (GAA) enzyme can confirm the diagnosis of Pompe’s disease.
- Genetic testing: Molecular genetic testing can identify mutations in the GAA gene associated with Pompe’s disease.
- Muscle biopsy: Examination of a muscle tissue sample may reveal glycogen accumulation and characteristic changes consistent with Pompe’s disease.
7. Pharmacokinetics (PK) and Pharmacodynamics (PD):
- Enzyme replacement therapy (ERT): The PK and PD of ERT, such as alglucosidase alfa, are crucial for understanding how these medications are absorbed, distributed, metabolized, and exert their therapeutic effects. ERT aims to supplement the deficient GAA enzyme and reduce glycogen accumulation in cells.
8. Pharmacological Treatment of Pompe’s Disease:
- Enzyme replacement therapy (ERT): Alglucosidase alfa, administered intravenously, is the mainstay of treatment for Pompe’s disease. ERT helps improve muscle strength, cardiac function, and respiratory function by reducing glycogen accumulation in tissues.
- Supportive therapy: Physical therapy, occupational therapy, and respiratory therapy can help manage symptoms and improve quality of life.
9. Non-pharmacological Treatment:
- Respiratory support: Mechanical ventilation or non-invasive ventilation may be necessary to manage respiratory complications, especially in individuals with severe muscle weakness.
- Nutritional support: Adequate nutrition and hydration are essential for maintaining overall health and supporting muscle function.
10. Conclusion: Pompe’s disease is a rare genetic disorder characterized by the accumulation of glycogen in cells, leading to progressive muscle weakness and other complications. Early diagnosis and prompt initiation of treatment, such as enzyme replacement therapy, are crucial for managing Pompe’s disease and improving outcomes. Additionally, supportive therapies and interventions can help alleviate symptoms and enhance the quality of life for individuals living with Pompe’s disease. Genetic counseling and testing are recommended for individuals with a family history of Pompe’s disease or carriers of the GAA gene mutation to assess the risk of passing the condition to their offspring.