Understanding Coronary Artery Disease (CAD): A Comprehensive Guide
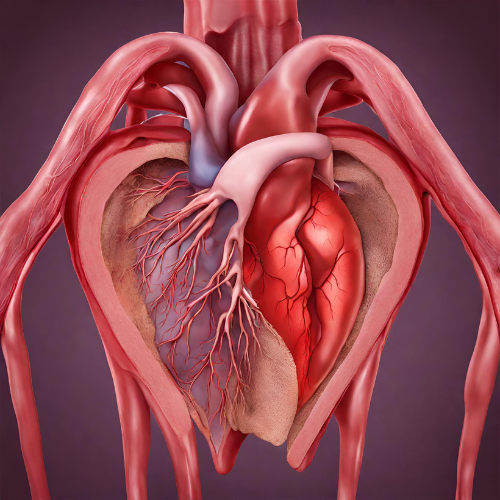
What is Coronary Artery Disease (CAD)? Coronary Artery Disease (CAD) is a common type of heart disease characterized by the narrowing or blockage of the coronary arteries, the blood vessels that supply oxygen-rich blood to the heart muscle. CAD is often caused by the buildup of plaque—a combination of cholesterol, fat, calcium, and other substances—inside the coronary arteries, leading to reduced blood flow to the heart.
Types of Coronary Artery Disease:
- Atherosclerosis: The most common form of CAD, involving the gradual buildup of plaque within the coronary arteries, leading to narrowing and obstruction of blood flow.
- Coronary Artery Spasm: In some cases, the coronary arteries may experience spasms or contractions, leading to temporary narrowing and reduced blood flow to the heart.
- Coronary Microvascular Disease: This type of CAD affects the small arteries and arterioles of the heart, impairing blood flow despite the absence of significant blockages in the main coronary arteries.
Symptoms of Coronary Artery Disease:
- Chest pain or discomfort (angina), typically described as pressure, squeezing, or tightness in the chest
- Shortness of breath, especially during physical exertion or emotional stress
- Fatigue
- Weakness
- Nausea
- Dizziness
- Sweating
Causes of Coronary Artery Disease: Coronary Artery Disease develops over time due to a combination of factors, including:
- Atherosclerosis: The buildup of plaque within the coronary arteries, often triggered by high cholesterol, high blood pressure, smoking, diabetes, and other risk factors.
- Endothelial dysfunction: Damage to the inner lining of the blood vessels, which can lead to inflammation and plaque formation.
- Risk factors: Smoking, high blood pressure, high cholesterol, obesity, sedentary lifestyle, diabetes, family history of heart disease, and age are all known risk factors for CAD.
Risk Factors for Coronary Artery Disease:
- Smoking: Cigarette smoking is a significant risk factor for CAD, increasing the risk of plaque buildup and blood vessel damage.
- High cholesterol: Elevated levels of LDL cholesterol (“bad” cholesterol) and low levels of HDL cholesterol (“good” cholesterol) contribute to plaque formation and arterial narrowing.
- High blood pressure: Hypertension puts added stress on the heart and blood vessels, increasing the risk of CAD and other cardiovascular complications.
- Diabetes: Diabetes is associated with insulin resistance, inflammation, and abnormal lipid metabolism, all of which contribute to CAD development.
- Family history: A family history of CAD or premature heart disease increases the likelihood of developing the condition.
- Age: The risk of CAD increases with age, particularly for men over 45 and women over 55.
Diagnosis of Coronary Artery Disease: Diagnosing CAD may involve:
- Medical history and physical examination
- Electrocardiogram (ECG or EKG) to measure electrical activity in the heart
- Stress tests to assess heart function during physical exertion
- Coronary angiography to visualize the coronary arteries and detect blockages
- Cardiac imaging tests such as echocardiography, CT scan, or MRI to evaluate heart structure and function
Pharmacokinetics and Pharmacodynamics: Pharmacokinetics refers to how medications are absorbed, distributed, metabolized, and excreted by the body, while pharmacodynamics refers to how medications exert their effects. In the treatment of CAD, pharmacological interventions aim to reduce symptoms, prevent complications, and improve overall cardiovascular health.
Pharmacological Treatment:
- Antiplatelet agents: Medications such as aspirin or clopidogrel to prevent blood clot formation and reduce the risk of heart attack and stroke.
- Statins: Cholesterol-lowering medications that help reduce LDL cholesterol levels and stabilize plaque within the coronary arteries.
- Beta-blockers: Drugs that decrease heart rate and blood pressure, reducing the heart’s workload and improving blood flow to the heart.
- ACE inhibitors or ARBs: Medications that help relax blood vessels, lower blood pressure, and improve heart function in patients with CAD and heart failure.
- Nitroglycerin: A vasodilator medication that helps relieve angina symptoms by relaxing and widening blood vessels, increasing blood flow to the heart.
Non-Pharmacological Treatment:
- Lifestyle modifications: Adopting a heart-healthy lifestyle, including regular exercise, a balanced diet low in saturated fats and cholesterol, smoking cessation, and stress management.
- Cardiac rehabilitation: Structured exercise programs, education, and counseling to help patients with CAD improve cardiovascular fitness, manage risk factors, and reduce the risk of future heart events.
- Revascularization procedures: Invasive procedures such as angioplasty with stent placement or coronary artery bypass grafting (CABG) may be necessary to restore blood flow to the heart in cases of severe coronary artery blockage.
Conclusion: Coronary Artery Disease is a common and serious condition that requires ongoing management and lifestyle modifications to reduce the risk of complications such as heart attack, stroke, and heart failure. By understanding the causes, symptoms, risk factors, diagnosis, and treatment options for CAD, individuals can take proactive steps to protect their heart health and improve their overall well-being. If you or someone you know experiences symptoms suggestive of CAD, it is essential to seek medical attention promptly for evaluation and appropriate management. Early detection and intervention can help prevent the progression of CAD and improve long-term outcomes for affected individuals.