Deciphering Chronic Lymphocytic Leukemia: Shedding Light on a Complex Blood Disorder
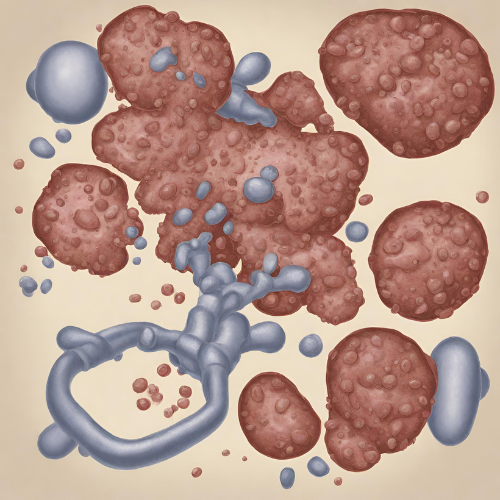
What is Chronic Lymphocytic Leukemia (CLL)? Chronic lymphocytic leukemia (CLL) is a type of cancer that affects the blood and bone marrow, causing an overproduction of abnormal lymphocytes, a type of white blood cell. These abnormal cells accumulate in the blood and lymphoid tissues, interfering with normal blood cell production and immune function. CLL is typically a slow-progressing disease, and many individuals may not require treatment for years after diagnosis.
Types of Chronic Lymphocytic Leukemia: CLL can be classified based on the presence or absence of certain genetic mutations and other factors:
- IgVH Mutational Status: CLL cells may have mutated (M-CLL) or unmutated (UM-CLL) immunoglobulin heavy-chain variable region genes, which can affect disease progression and treatment response.
- ZAP-70 Expression: High expression of the protein ZAP-70 is associated with more aggressive disease and poorer prognosis in CLL.
- FISH Analysis: Fluorescence in situ hybridization (FISH) testing can identify chromosomal abnormalities such as del(17p), del(11q), and trisomy 12, which may influence treatment decisions and prognosis in CLL.
Symptoms of Chronic Lymphocytic Leukemia: Many individuals with CLL may not experience any symptoms in the early stages of the disease. Common symptoms of CLL may include:
- Enlarged lymph nodes, particularly in the neck, armpits, or groin.
- Fatigue and weakness.
- Easy bruising or bleeding.
- Night sweats.
- Fever and recurrent infections.
- Unexplained weight loss.
- Abdominal discomfort or fullness.
- Shortness of breath.
Causes of Chronic Lymphocytic Leukemia: The exact cause of CLL is unknown, but it is believed to result from a combination of genetic, environmental, and immune system factors. Risk factors for CLL may include:
- Age: CLL is most commonly diagnosed in older adults, with the average age at diagnosis being around 70 years.
- Family history: Having a first-degree relative (parent, sibling, or child) with CLL or other lymphoid malignancies increases the risk of developing the disease.
- Exposure to certain chemicals or radiation: Prolonged exposure to chemicals such as benzene or certain pesticides, as well as ionizing radiation, may increase the risk of developing CLL.
Risk Factors for Chronic Lymphocytic Leukemia: Several factors may increase the risk of developing CLL, including:
- Age: CLL is most commonly diagnosed in older adults, with the average age at diagnosis being around 70 years.
- Gender: Men are slightly more likely to develop CLL than women.
- Family history: Having a first-degree relative (parent, sibling, or child) with CLL or other lymphoid malignancies increases the risk of developing the disease.
- Race and ethnicity: CLL is more common in Caucasians than in other racial or ethnic groups.
Diagnosis of Chronic Lymphocytic Leukemia: Diagnosis of CLL typically involves a combination of medical history, physical examination, laboratory tests, and imaging studies. Common diagnostic tests for CLL may include:
- Complete blood count (CBC) with differential: To evaluate the number and types of blood cells, including lymphocytes.
- Flow cytometry: To analyze the characteristics of lymphocytes and detect abnormal cell markers.
- Bone marrow biopsy: To examine the bone marrow for the presence of abnormal cells and assess disease progression.
Pharmacokinetics and Pharmacodynamics: Pharmacological treatment for CLL aims to slow disease progression, reduce symptoms, and improve overall survival. These medications may vary in their absorption, distribution, metabolism, and excretion, as well as their mechanisms of action within the body.
Pharmacological Treatment:
- Chemotherapy: Drugs such as fludarabine, cyclophosphamide, and rituximab may be used alone or in combination to kill cancer cells and slow disease progression.
- Targeted therapy: Drugs such as ibrutinib, venetoclax, or idelalisib target specific pathways involved in CLL cell growth and survival, leading to improved outcomes in certain patients.
- Immunotherapy: Monoclonal antibodies such as rituximab, obinutuzumab, or ofatumumab stimulate the immune system to recognize and destroy CLL cells.
Non-Pharmacological Treatment:
- Watchful waiting: In asymptomatic or early-stage CLL, active surveillance may be recommended, with treatment initiated only when the disease progresses or symptoms worsen.
- Supportive care: Measures such as blood transfusions, growth factor injections, and antibiotics may be used to manage complications such as anemia, low platelet counts, or infections.
- Stem cell transplant: In younger, fit patients with high-risk CLL, allogeneic stem cell transplant may be considered as a potentially curative treatment option.
Conclusion: Chronic lymphocytic leukemia is a complex blood cancer characterized by the overproduction of abnormal lymphocytes. While CLL is typically a slow-progressing disease, it can cause a wide range of symptoms and complications that significantly impact quality of life. With advances in diagnosis and treatment, many individuals with CLL are living longer and enjoying a better quality of life than ever before. Ongoing research and clinical trials are essential for improving outcomes and finding new therapies for this challenging disease. By raising awareness, advocating for research funding, and providing support to individuals and families affected by CLL, we can continue to make strides towards better treatments and ultimately a cure for this condition.