Demystifying Diabetes Mellitus: Understanding Symptoms, Causes, and Management
What is Diabetes Mellitus? Diabetes mellitus, commonly referred to as diabetes, is a chronic metabolic disorder characterized by elevated blood sugar levels (hyperglycemia) resulting from defects in insulin production, insulin action, or both. Insulin, a hormone produced by the pancreas, plays a crucial role in regulating blood sugar levels and facilitating the uptake of glucose into cells for energy.
Types of Diabetes Mellitus:
- Type 1 Diabetes: Results from the immune-mediated destruction of insulin-producing beta cells in the pancreas, leading to absolute insulin deficiency. It often develops in childhood or adolescence and requires lifelong insulin therapy for management.
- Type 2 Diabetes: Occurs when the body becomes resistant to the effects of insulin or fails to produce enough insulin to meet its needs. It is more common in adults and is often associated with obesity, sedentary lifestyle, and genetic predisposition.
- Gestational Diabetes: Develops during pregnancy and is characterized by elevated blood sugar levels that may pose risks to both the mother and baby. It typically resolves after childbirth but increases the risk of developing type 2 diabetes later in life.
Symptoms of Diabetes Mellitus:
- Excessive thirst (polydipsia)
- Frequent urination (polyuria)
- Increased hunger (polyphagia)
- Unexplained weight loss
- Fatigue and weakness
- Blurred vision
- Slow wound healing
- Recurrent infections, particularly of the skin, gums, or urinary tract
Causes of Diabetes Mellitus:
- Type 1 Diabetes:
- Autoimmune destruction of pancreatic beta cells
- Genetic predisposition
- Environmental factors, such as viral infections or dietary factors, may trigger the autoimmune response.
- Type 2 Diabetes:
- Insulin resistance: Reduced sensitivity of cells to insulin, often associated with obesity, physical inactivity, and genetic factors.
- Beta-cell dysfunction: Gradual decline in insulin production and secretion by pancreatic beta cells due to metabolic stress and genetic factors.
- Lifestyle factors: Sedentary lifestyle, unhealthy diet high in refined carbohydrates and saturated fats, and excessive calorie intake contribute to the development of type 2 diabetes.
Risk Factors for Diabetes Mellitus:
- Family history of diabetes
- Obesity or overweight
- Sedentary lifestyle
- Age (risk increases with age, particularly after 45 years)
- Ethnicity (higher prevalence among certain racial and ethnic groups)
- Gestational diabetes or polycystic ovary syndrome (PCOS)
- History of cardiovascular disease or metabolic syndrome
Diagnosis of Diabetes Mellitus:
- Fasting Plasma Glucose Test: Measures blood sugar levels after an overnight fast.
- Oral Glucose Tolerance Test (OGTT): Measures blood sugar levels before and after consuming a glucose-rich beverage.
- Hemoglobin A1c (HbA1c) Test: Reflects average blood sugar levels over the past two to three months.
Management of Diabetes Mellitus:
- Lifestyle Modifications:
- Healthy diet: Emphasize whole grains, fruits, vegetables, lean proteins, and healthy fats. Limit intake of refined carbohydrates, sugary beverages, and high-fat foods.
- Regular physical activity: Aim for at least 150 minutes of moderate-intensity aerobic activity per week, along with muscle-strengthening activities on two or more days per week.
- Weight management: Achieve and maintain a healthy weight through a balanced diet and regular exercise.
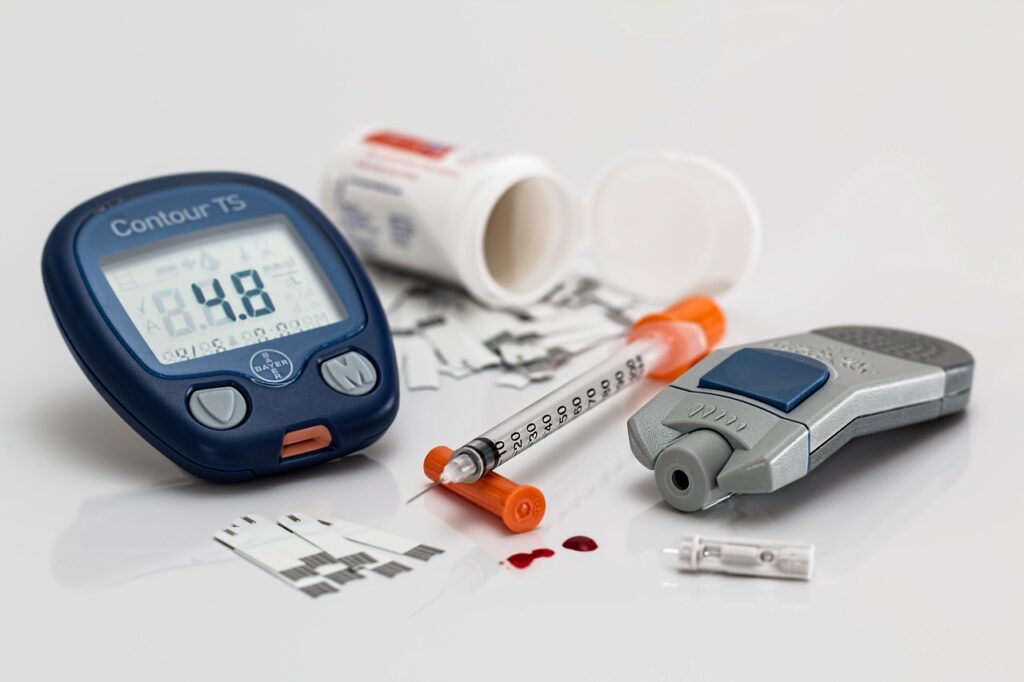
- Medication Therapy:
- Type 1 Diabetes: Requires lifelong insulin therapy delivered via injections or insulin pump.
- Type 2 Diabetes: Oral medications, injectable medications (such as GLP-1 receptor agonists or insulin), or a combination of both may be prescribed to lower blood sugar levels and improve insulin sensitivity.
- Blood Sugar Monitoring:
- Regular monitoring of blood sugar levels using a glucometer helps individuals with diabetes track their progress and make necessary adjustments to their treatment plan.
- Regular Medical Care:
- Routine medical check-ups, including eye exams, foot exams, and kidney function tests, are essential for monitoring complications and adjusting treatment as needed.
Conclusion: Diabetes mellitus is a chronic condition that requires lifelong management to prevent complications and maintain optimal health. By understanding the symptoms, causes, risk factors, and management strategies for diabetes, individuals can take proactive steps to control their blood sugar levels, reduce the risk of complications, and improve their overall quality of life. If you suspect you have diabetes or have been diagnosed with diabetes, it’s essential to work closely with your healthcare provider to develop a personalized treatment plan tailored to your needs and goals. With proper self-care and medical management, individuals with diabetes can live healthy, fulfilling lives.