Understanding Familial Dilated Cardiomyopathy: Causes, Symptoms, Treatment, and Management
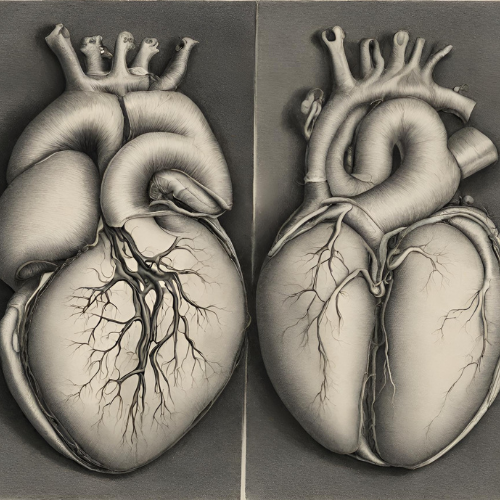
What is Familial Dilated Cardiomyopathy (DCM)? Familial dilated cardiomyopathy (DCM) is a genetic heart disorder characterized by the enlargement (dilation) and weakening of the heart’s main pumping chamber, the left ventricle. This condition impairs the heart’s ability to pump blood efficiently to the body, leading to symptoms of heart failure and an increased risk of complications such as arrhythmias and sudden cardiac death. Familial DCM is inherited in an autosomal dominant pattern, meaning that a person only needs to inherit one copy of the defective gene from either parent to develop the condition.
Symptoms of Familial Dilated Cardiomyopathy: The symptoms of familial dilated cardiomyopathy can vary widely among affected individuals and may include:
- Shortness of breath (dyspnea) during physical activity or at rest.
- Fatigue and weakness.
- Swelling (edema) in the legs, ankles, or feet.
- Rapid or irregular heartbeat (palpitations).
- Chest pain or discomfort.
- Dizziness or lightheadedness.
- Fainting or syncope.
- Reduced ability to exercise or perform daily activities.
Causes and Risk Factors: Familial dilated cardiomyopathy is primarily caused by mutations in genes that regulate the structure and function of the heart muscle. These genetic mutations disrupt the normal contraction and relaxation of heart muscle cells, leading to dilation and weakening of the heart chambers. Risk factors for familial DCM include:
- Family history of dilated cardiomyopathy or sudden cardiac death.
- Inherited genetic mutations associated with familial DCM.
- Certain medical conditions or syndromes that predispose to cardiomyopathy, such as muscular dystrophy or metabolic disorders.
- Exposure to cardiotoxic substances, such as alcohol, certain chemotherapy drugs, or illicit drugs.
Diagnosis: Diagnosing familial dilated cardiomyopathy typically involves a combination of clinical evaluation, imaging tests, and genetic testing. Diagnostic tests may include:
- Physical examination and medical history.
- Electrocardiogram (ECG or EKG) to evaluate the heart’s electrical activity.
- Echocardiogram to assess the size, shape, and function of the heart chambers.
- Cardiac magnetic resonance imaging (MRI) for detailed imaging of the heart muscle.
- Genetic testing to identify mutations in genes associated with familial DCM.
Treatment Options: Treatment for familial dilated cardiomyopathy focuses on managing symptoms, slowing disease progression, and reducing the risk of complications. Common treatment approaches may include:
- Medications:
- ACE inhibitors, beta-blockers, or angiotensin receptor blockers to improve heart function and reduce symptoms.
- Diuretics to relieve fluid buildup and reduce swelling.
- Anticoagulants or antiplatelet medications to prevent blood clots.
- Implantable devices:
- Implantable cardioverter-defibrillator (ICD) to monitor heart rhythm and deliver electrical shocks if life-threatening arrhythmias occur.
- Cardiac resynchronization therapy (CRT) to improve heart function and reduce symptoms in some patients.
- Heart transplant:
- For severe cases of familial DCM that do not respond to medical therapy, heart transplantation may be considered as a last resort.
Management and Lifestyle Modifications: In addition to medical treatment, individuals with familial dilated cardiomyopathy can take steps to manage their condition and improve their quality of life:
- Follow a heart-healthy diet low in sodium and saturated fats.
- Maintain a healthy weight and participate in regular physical activity as tolerated.
- Avoid smoking and limit alcohol intake.
- Monitor and manage other medical conditions, such as hypertension or diabetes.
- Attend regular follow-up appointments with a cardiologist to monitor disease progression and adjust treatment as needed.
- Educate family members about the genetic nature of familial DCM and encourage screening for early detection and intervention.
Conclusion: Familial dilated cardiomyopathy is a genetic heart condition characterized by the enlargement and weakening of the heart muscle, leading to symptoms of heart failure and an increased risk of complications. While there is currently no cure for familial DCM, advances in medical treatment and genetic testing have improved outcomes for affected individuals. With early diagnosis, personalized treatment, and lifestyle modifications, individuals with familial dilated cardiomyopathy can effectively manage their condition and lead fulfilling lives. If you or a family member have symptoms suggestive of familial DCM or have a family history of the condition, seek medical evaluation and genetic counseling for appropriate diagnosis and management.