Understanding Fibroids: Types, Symptoms, Causes, Diagnosis, Treatment, and Management
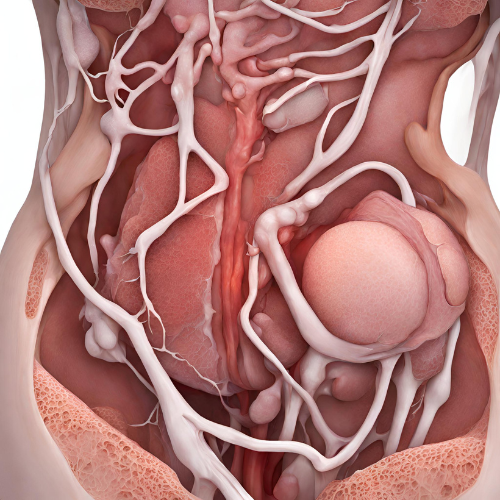
What are Fibroids? Fibroids, also known as uterine leiomyomas or myomas, are noncancerous growths that develop in the uterus. These tumors are made of muscle cells and fibrous tissue and can vary in size, ranging from tiny seedlings that are undetectable to large masses that can distort the shape of the uterus. Fibroids can develop inside the uterus (intramural), on the outer surface of the uterus (subserosal), or within the uterine cavity (submucosal).
Types of Fibroids:
- Intramural fibroids: These are the most common type of fibroids and develop within the muscular wall of the uterus.
- Subserosal fibroids: These fibroids grow on the outer surface of the uterus and can protrude into the pelvic cavity.
- Submucosal fibroids: These fibroids develop in the inner lining of the uterus and can protrude into the uterine cavity.
Symptoms of Fibroids: Fibroids may not cause any symptoms in some women and may be discovered incidentally during a pelvic exam or imaging study. However, for others, fibroids can cause the following symptoms:
- Heavy menstrual bleeding (menorrhagia).
- Prolonged menstrual periods or bleeding between periods.
- Pelvic pain or pressure.
- Frequent urination or difficulty emptying the bladder.
- Constipation or difficulty with bowel movements.
- Lower back pain.
- Enlargement of the lower abdomen.
- Pain during intercourse.
Causes and Risk Factors: The exact cause of fibroids is not known, but several factors may contribute to their development, including:
- Hormonal factors: Estrogen and progesterone, hormones that stimulate the growth of the uterine lining during each menstrual cycle, may promote the growth of fibroids.
- Genetic factors: A family history of fibroids may increase the risk of developing the condition.
- Race: African American women are at a higher risk of developing fibroids and may experience more severe symptoms compared to women of other racial or ethnic groups.
- Age: Fibroids typically develop during a woman’s reproductive years and may shrink after menopause due to a decrease in hormone levels.
Diagnosis: Fibroids may be diagnosed during a routine pelvic exam, but additional tests may be needed to confirm the diagnosis and evaluate the size and location of the fibroids. Diagnostic tests may include:
- Pelvic ultrasound: This imaging test uses sound waves to create pictures of the uterus and other pelvic organs to detect the presence of fibroids.
- Magnetic resonance imaging (MRI): An MRI scan provides detailed images of the uterus and can help determine the size, number, and location of fibroids.
- Hysteroscopy: This minimally invasive procedure involves inserting a thin, lighted tube with a camera (hysteroscope) through the vagina and cervix to visualize the inside of the uterus and detect submucosal fibroids.
Treatment Options: Treatment for fibroids depends on the size, location, and severity of symptoms, as well as the patient’s age and desire for future fertility. Treatment options may include:
- Watchful waiting: If fibroids are small and not causing symptoms, regular monitoring may be recommended without immediate treatment.
- Medications:
- Nonsteroidal anti-inflammatory drugs (NSAIDs) to relieve pelvic pain and discomfort.
- Hormonal medications such as birth control pills, hormonal IUDs, or gonadotropin-releasing hormone (GnRH) agonists to help regulate menstrual bleeding and reduce fibroid size.
- Minimally invasive procedures:
- Uterine artery embolization (UAE) to block the blood supply to fibroids and shrink them.
- Myomectomy to surgically remove fibroids while preserving the uterus, which may be recommended for women who want to preserve fertility.
- Surgical procedures:
- Hysterectomy to remove the uterus, which is considered a definitive treatment for fibroids but may not be suitable for women who want to have children in the future.
- Endometrial ablation to destroy the lining of the uterus and reduce menstrual bleeding, which may be recommended for women with submucosal fibroids and heavy menstrual bleeding.
Management and Lifestyle Modifications: In addition to medical treatment, lifestyle modifications may help manage symptoms and reduce the risk of fibroid growth:
- Maintain a healthy weight and engage in regular physical activity.
- Eat a balanced diet rich in fruits, vegetables, whole grains, and lean proteins.
- Manage stress through relaxation techniques such as meditation, yoga, or deep breathing exercises.
- Avoid alcohol and caffeine, which may exacerbate symptoms of fibroids.
- Practice good pelvic floor health and perform pelvic floor exercises to improve pelvic muscle strength and support.
Conclusion: Fibroids are common noncancerous growths that develop in the uterus and can cause a variety of symptoms, including heavy menstrual bleeding