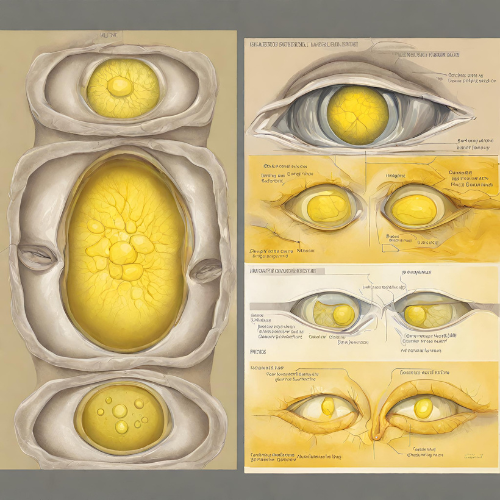
What is Jaundice? Jaundice is a medical condition characterized by yellowing of the skin, mucous membranes, and the whites of the eyes. It occurs when there is an excess buildup of bilirubin in the blood, a yellow pigment produced by the breakdown of red blood cells. Jaundice can be a sign of an underlying health problem affecting the liver, gallbladder, or bile ducts.
Types of Jaundice:
- Hepatocellular Jaundice: This type of jaundice occurs when there is liver damage or dysfunction, leading to impaired bilirubin processing and clearance.
- Hemolytic Jaundice: Hemolytic jaundice results from increased breakdown of red blood cells, leading to elevated levels of bilirubin in the bloodstream.
- Obstructive Jaundice: Obstructive jaundice occurs when there is a blockage in the bile ducts, preventing the flow of bile and causing bilirubin buildup in the blood.
Symptoms of Jaundice:
- Yellowing of the skin, eyes, and mucous membranes
- Dark urine
- Pale stools
- Itching (pruritus)
- Fatigue and weakness
- Abdominal pain or discomfort
- Nausea and vomiting
- Fever (in some cases)
Causes of Jaundice:
- Liver Disorders: Hepatitis, cirrhosis, alcoholic liver disease, and liver cancer can impair liver function and lead to jaundice.
- Hemolytic Disorders: Conditions such as hemolytic anemia, sickle cell disease, and thalassemia cause increased breakdown of red blood cells, resulting in hemolytic jaundice.
- Bile Duct Obstruction: Gallstones, tumors, or inflammation of the bile ducts can block the flow of bile, leading to obstructive jaundice.
- Infections: Viral hepatitis (hepatitis A, B, C, etc.) and other infections affecting the liver can cause jaundice.
- Medications: Certain medications, such as acetaminophen, can cause liver damage and jaundice in some individuals.
Risk Factors for Jaundice:
- Alcohol abuse
- Chronic liver disease
- Gallstones or bile duct disorders
- Family history of liver disease
- Exposure to hepatitis viruses
- Certain medications or herbal supplements
Diagnosis of Jaundice:
- Physical Examination: A healthcare provider will examine the skin, eyes, and abdomen for signs of jaundice and other symptoms.
- Blood Tests: Blood tests, including liver function tests and bilirubin levels, can help diagnose the underlying cause of jaundice.
- Imaging Studies: Ultrasound, CT scan, or MRI may be performed to evaluate the liver, bile ducts, and gallbladder for abnormalities.
- Liver Biopsy: In some cases, a liver biopsy may be necessary to obtain a tissue sample for further evaluation.
Treatment of Jaundice:
- Management of Underlying Cause: Treatment depends on the underlying cause of jaundice and may include medications, lifestyle changes, or surgical intervention.
- Supportive Care: Symptomatic treatment may include rest, hydration, and pain management to alleviate discomfort and fatigue.
- Bile Duct Clearance: Obstructive jaundice may require procedures such as endoscopic retrograde cholangiopancreatography (ERCP) or surgery to remove bile duct blockages.
- Liver Transplant: In severe cases of liver failure or advanced liver disease, liver transplant surgery may be considered as a treatment option.
Non-Pharmacological Treatment:
- Dietary Changes: Avoiding alcohol and adopting a healthy diet rich in fruits, vegetables, and whole grains can support liver health.
- Hydration: Drinking plenty of fluids helps flush toxins from the body and promotes liver function.
- Avoiding Hepatotoxic Substances: Avoiding exposure to hepatotoxic substances, such as certain medications and chemicals, can help prevent liver damage and jaundice.
Conclusion: Jaundice is a common medical condition characterized by yellowing of the skin and eyes due to elevated levels of bilirubin in the blood. While jaundice itself is not a disease, it can be a symptom of underlying liver, gallbladder, or bile duct disorders. Early diagnosis and treatment of the underlying cause are crucial for managing jaundice and preventing complications. If you or someone you know experiences symptoms of jaundice, it is important to seek medical attention for proper evaluation and management.