Oophorectomy is a surgical procedure involving the removal of one or both ovaries. This procedure may be performed for various medical reasons, including the treatment or prevention of ovarian cancer, endometriosis, ovarian cysts, or as part of gender-affirming surgery. Understanding the indications, types, risks, and potential outcomes of oophorectomy is essential for individuals considering this treatment option.
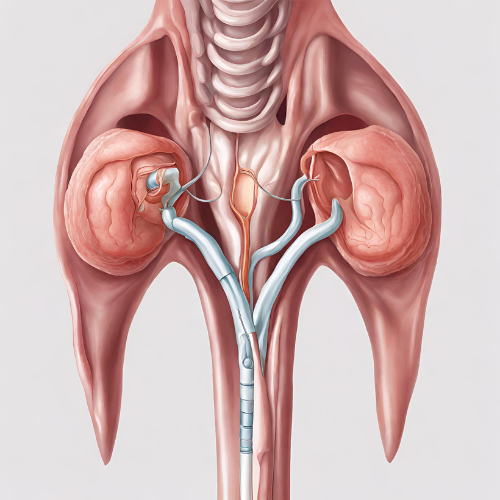
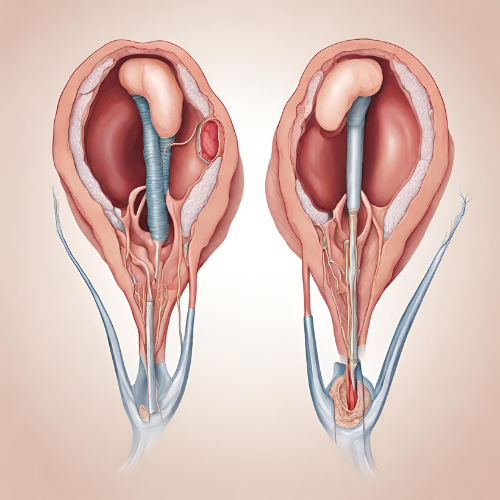
What is Oophorectomy? Oophorectomy, also known as ovarian removal surgery, is a surgical procedure that involves the removal of one or both ovaries. The ovaries are reproductive organs responsible for producing eggs (ova) and female sex hormones, including estrogen and progesterone. Oophorectomy may be performed as a standalone procedure or in conjunction with other gynecological surgeries, such as hysterectomy (removal of the uterus).
Types of Oophorectomy:
- Unilateral Oophorectomy: Removal of one ovary while preserving the other.
- Bilateral Oophorectomy: Removal of both ovaries.
Indications for Oophorectomy: Oophorectomy may be recommended for various medical reasons, including:
- Ovarian Cancer: Treatment of ovarian cancer or as a preventive measure in individuals at high risk of developing ovarian cancer.
- Endometriosis: Management of severe endometriosis-related pain or symptoms that do not respond to other treatments.
- Ovarian Cysts: Removal of large or persistent ovarian cysts that cause symptoms or complications.
- Hormone-related Disorders: Treatment of hormone-sensitive conditions, such as estrogen-receptor-positive breast cancer or polycystic ovary syndrome (PCOS).
- Gender-Affirming Surgery: As part of gender transition for transgender individuals seeking to align their physical characteristics with their gender identity.
Risks and Complications: While oophorectomy is generally considered safe, it carries certain risks and potential complications, including:
- Surgical Risks: Infection, bleeding, blood clots, anesthesia complications, and damage to surrounding organs or tissues.
- Menopausal Symptoms: Removal of both ovaries results in surgical menopause, leading to symptoms such as hot flashes, night sweats, vaginal dryness, and mood changes.
- Hormone Imbalance: Disruption of hormonal balance, particularly estrogen deficiency, which can increase the risk of osteoporosis, cardiovascular disease, and cognitive changes.
- Long-Term Health Effects: Increased risk of cardiovascular disease, osteoporosis, and certain cancers associated with early or surgical menopause.
- Psychological Impact: Emotional distress, grief, or loss associated with the removal of reproductive organs, particularly in individuals who have not completed their family planning or experience changes in sexual function.
Diagnosis and Evaluation: The decision to undergo oophorectomy is based on individual medical history, symptoms, diagnostic tests, and discussions with healthcare providers. Diagnostic evaluations may include:
- Medical History: Assessment of symptoms, family history of cancer, hormone-related disorders, or previous gynecological surgeries.
- Imaging Studies: Pelvic ultrasound, magnetic resonance imaging (MRI), or computed tomography (CT) scans to evaluate ovarian cysts, tumors, or other abnormalities.
- Biopsy: Removal and analysis of tissue samples (biopsy) to diagnose ovarian cancer or evaluate suspicious ovarian masses.
Pharmacokinetics (PK) and Pharmacodynamics (PD): Oophorectomy does not involve pharmacokinetics or pharmacodynamics as it is a surgical procedure. However, hormone replacement therapy (HRT) may be prescribed postoperatively to manage menopausal symptoms and prevent long-term health consequences associated with estrogen deficiency.
Postoperative Care and Recovery: Following oophorectomy, individuals require postoperative care and monitoring to promote healing and manage potential complications. Postoperative care may include:
- Pain Management: Administration of pain medications to alleviate discomfort and promote mobility.
- Monitoring: Regular monitoring of vital signs, wound healing, and potential signs of complications, such as infection or bleeding.
- Hormone Replacement Therapy (HRT): Initiation of HRT, if indicated, to manage menopausal symptoms and reduce the risk of long-term health consequences associated with estrogen deficiency.
- Activity Restrictions: Temporary restrictions on physical activity, lifting heavy objects, or sexual intercourse to prevent strain on the surgical site and facilitate healing.
- Follow-Up Visits: Scheduled follow-up visits with healthcare providers to assess recovery, address concerns, and monitor hormone levels or other health indicators.
Conclusion: Oophorectomy is a surgical procedure involving the removal of one or both ovaries for various medical reasons, including ovarian cancer treatment, endometriosis management, or as part of gender-affirming surgery. While oophorectomy can effectively address certain health conditions, it carries risks and potential complications, particularly related to menopausal symptoms and hormone imbalance. Individuals considering oophorectomy should engage in thorough discussions with healthcare providers to weigh the benefits, risks, and potential long-term implications of the procedure.