Navigating the Maze of Crohn’s Disease: Unraveling the Challenges
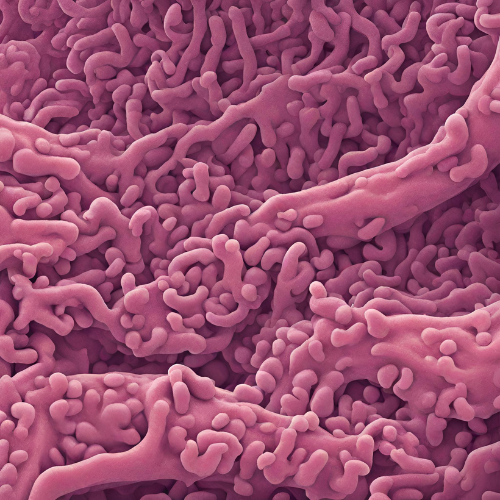
What is Crohn’s Disease? Crohn’s disease is a chronic inflammatory bowel disease (IBD) characterized by inflammation of the digestive tract. It can affect any part of the gastrointestinal (GI) tract, from the mouth to the anus, but most commonly involves the small intestine and the beginning of the large intestine (colon). Crohn’s disease is a lifelong condition that requires ongoing management and treatment.
Types of Crohn’s Disease: Crohn’s disease can be classified based on the location and pattern of inflammation:
- Ileocolitis: Inflammation occurs in the ileum (the end of the small intestine) and the colon.
- Ileitis: Inflammation is confined to the ileum.
- Gastroduodenal Crohn’s Disease: Inflammation affects the stomach and duodenum (the first part of the small intestine).
- Jejunoileitis: Inflammation is limited to the jejunum (the middle part of the small intestine).
- Crohn’s Colitis: Inflammation is limited to the colon.
Symptoms of Crohn’s Disease: Common symptoms of Crohn’s disease include:
- Abdominal pain and cramping.
- Diarrhea, sometimes bloody.
- Rectal bleeding.
- Fatigue.
- Unintended weight loss.
- Loss of appetite.
- Fever.
- Mouth sores.
- Perianal disease (abscesses, fistulas, fissures).
Causes of Crohn’s Disease: The exact cause of Crohn’s disease is unknown, but it is believed to involve a combination of genetic, environmental, and immune system factors. Possible causes and risk factors include:
- Genetic predisposition: Individuals with a family history of Crohn’s disease are at increased risk.
- Immune system dysfunction: Abnormal immune responses may trigger inflammation in the digestive tract.
- Environmental factors: Factors such as diet, smoking, and exposure to certain bacteria or viruses may contribute to the development of Crohn’s disease.
Risk Factors for Crohn’s Disease: Several factors may increase the risk of developing Crohn’s disease, including:
- Family history: Having a close relative with Crohn’s disease increases the risk.
- Age: Crohn’s disease can occur at any age, but it is most commonly diagnosed in people between the ages of 15 and 35.
- Ethnicity: Crohn’s disease is more common in Caucasians than in other ethnic groups.
- Smoking: Smoking increases the risk of developing Crohn’s disease and can worsen symptoms in people who already have the condition.
Diagnosis of Crohn’s Disease: Diagnosis of Crohn’s disease typically involves a combination of medical history, physical examination, and diagnostic tests, including:
- Blood tests: To check for signs of inflammation or anemia.
- Stool tests: To rule out infections or other causes of gastrointestinal symptoms.
- Colonoscopy or sigmoidoscopy: A procedure to examine the inside of the colon and obtain tissue samples for biopsy.
- Imaging tests: Such as CT scans or MRI scans, to assess the extent and severity of inflammation in the digestive tract.
Pharmacokinetics and Pharmacodynamics: Pharmacological treatment for Crohn’s disease aims to reduce inflammation, control symptoms, and prevent complications. These medications may vary in their absorption, distribution, metabolism, and excretion, as well as their mechanisms of action within the body.
Pharmacological Treatment:
- Anti-inflammatory drugs: Corticosteroids such as prednisone or budesonide may be used to reduce inflammation during flare-ups.
- Immunomodulators: Drugs such as azathioprine, mercaptopurine, or methotrexate help suppress the immune system to reduce inflammation and prevent disease progression.
- Biologic therapies: Monoclonal antibodies such as infliximab, adalimumab, or ustekinumab target specific proteins involved in the inflammatory process and can induce and maintain remission in Crohn’s disease.
Non-Pharmacological Treatment:
- Nutritional therapy: Some individuals with Crohn’s disease may benefit from dietary modifications, such as avoiding certain trigger foods or following a low-residue diet during flare-ups.
- Lifestyle modifications: Adopting a healthy lifestyle, including regular exercise, stress management, and smoking cessation, can help improve overall health and well-being in individuals with Crohn’s disease.
- Surgery: In severe cases of Crohn’s disease with complications such as strictures, fistulas, or abscesses, surgery may be necessary to remove diseased portions of the intestine or repair damaged tissue.
Conclusion: Crohn’s disease is a chronic inflammatory bowel disease that can have a significant impact on quality of life. With proper diagnosis, treatment, and ongoing management, many individuals with Crohn’s disease can achieve remission and lead fulfilling lives. It’s essential for individuals with Crohn’s disease to work closely with their healthcare providers to develop a personalized treatment plan that addresses their unique needs and goals. Through a combination of pharmacological and non-pharmacological interventions, individuals with Crohn’s disease can effectively manage their symptoms, reduce